All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the Lymphoma Coalition.
The Lymphoma Hub uses cookies on this website. They help us give you the best online experience. By continuing to use our website without changing your cookie settings, you agree to our use of cookies in accordance with our updated Cookie Policy
Introducing

Now you can personalise
your Lymphoma Hub experience!
Bookmark content to read later
Select your specific areas of interest
View content recommended for you
Find out moreThe Lymphoma Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the Lymphoma Hub cannot guarantee the accuracy of translated content. The Lymphoma Hub and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
ASH 2016 | Prognostic Value of Baseline Quantitative PET Metrics for Patients with Unfavorable Early Stage Hodgkin Lymphoma Enrolled in the Standard Arm of the EORTC/Lysa/FIL H10 Trial
Bookmark this article
The 58th Annual Meeting & Exposition of the American Society of Hematology’s (ASH) took place in San Diego, CA, and on December 3rd, Anne Ségolène Cottereau, MD, from the Hôpital Henri Mondor, Créteil, France, presented analysis of data from the H10 EORTC/LYSA/FIL trial.
The authors set out to assess baseline FDG PET/CT scans to assay prognostic value of two quantitative PET measurements in 128 patients randomly selected from 352 patients in the unfavorable group of the standard arm. The two measurements assessed were total metabolic tumor volume (TMTV) and total lesion glycolysis (TLG), and standard treatment was 4 cycles of ABVD with PET2 after 2 cycles of ABVD.
Highlights:
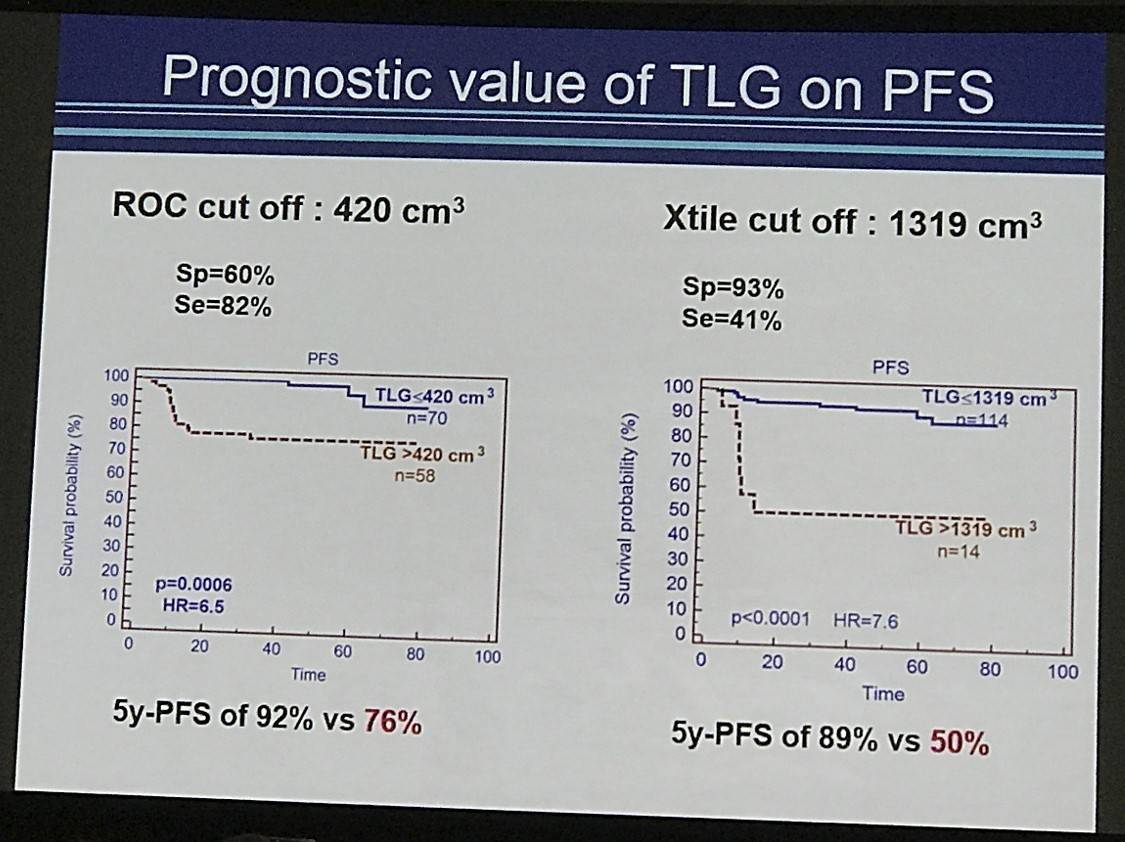
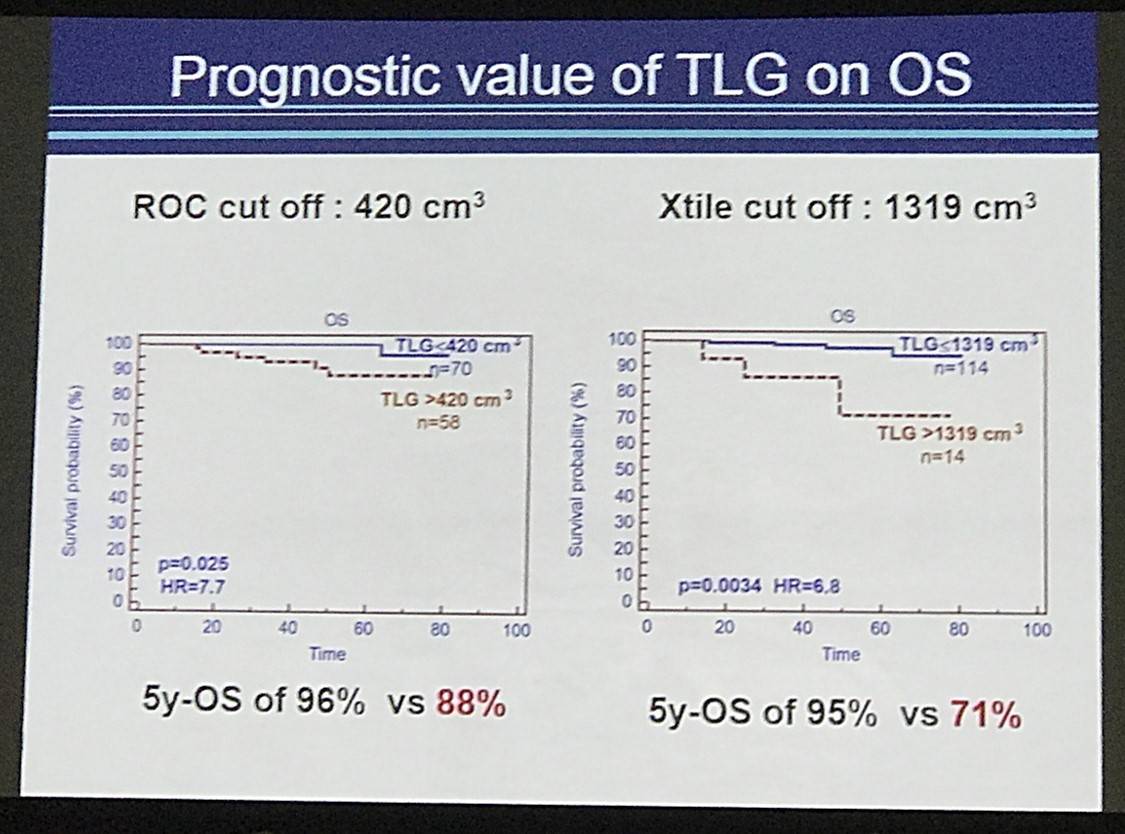
- Strongest quantitative PET predictor was TLG41% for PFS (P=0.0006, HR=6.5) and OS (P=0.025 HR=7.7)
- TMTV41% was a worse predictor with both PFS (P=0.0099, HR= 3.26) and OS (P=0.022, HR= 2.8 than TLG41%.
- In multivariate analysis only TLG41% was a significant predictor of PFS and OS
- Overall 5yr PFS = 84%, 5yr OS = 92%
- High TLG41% 5yr PFS = 76% vs lower TLG41% = 92%
- High TLG41% 5yr OS = 88% vs lower TLG41% = 96%
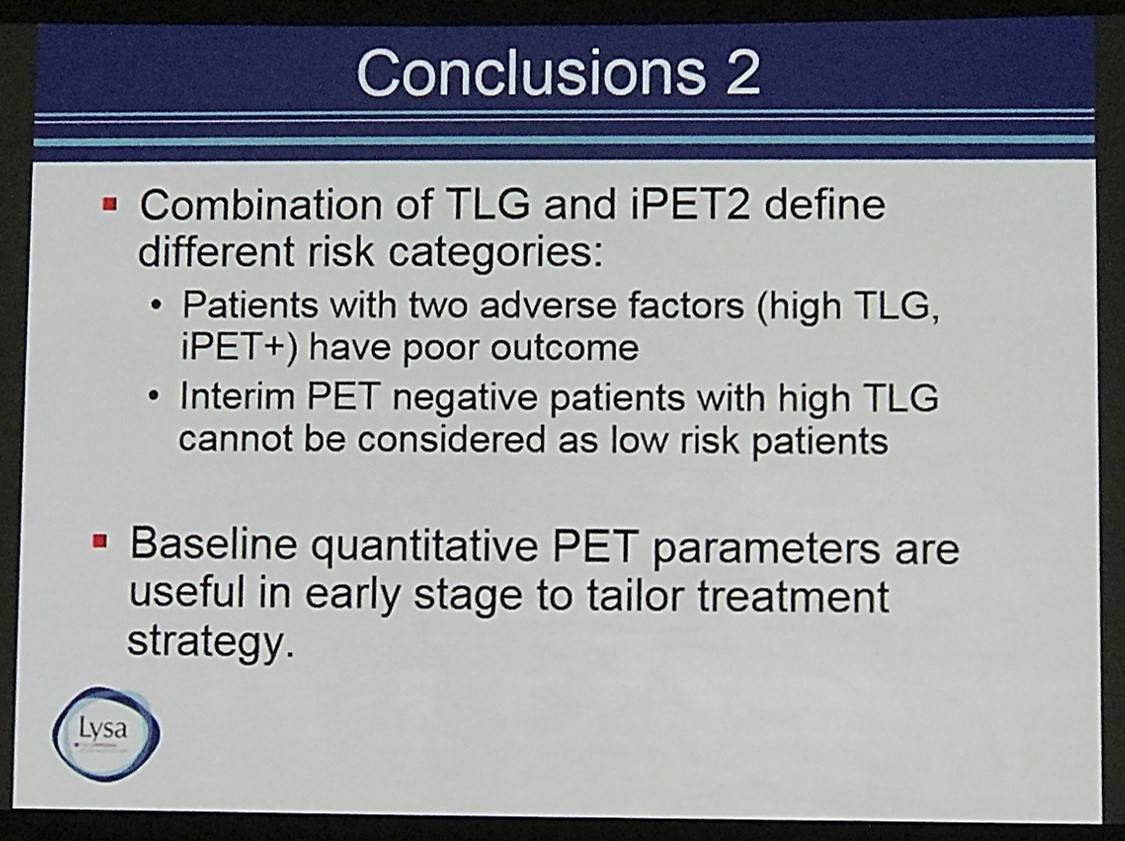
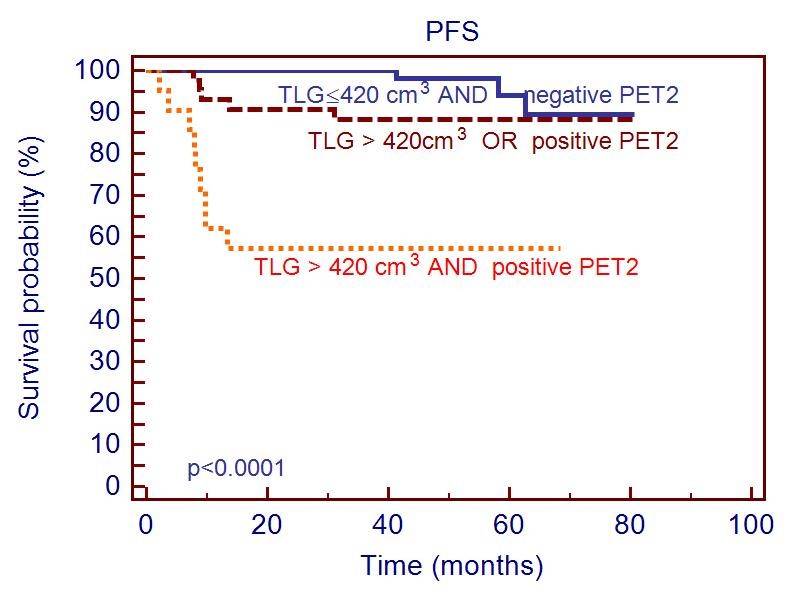
- Combining TLG41% and interim PET resulted in 3 prognostic categories:
- Poor outcome with 5yr PFS 57% = positive PET2 and high TLG41%
- Intermediate with 5yr PFS 88%
- Good outcome with 5yr PFS 92% = negative PET2 and low TLG41%
Anne Ségolène Cottereau concluded by suggesting that including TLG41% status in prognostic may decrease the false positive rate of PET2. Furthermore, TLD was suggested to be an independent prognostic indicator in early stage HL and could be used to target treatment intensification.
Abstract:
Objective: Baseline quantitative PET parameters measuring tumour burden and metabolism are proposed as early prognosticators of outcome in different lymphoma subtypes. It has been shown that in advanced stage Hodgkin lymphoma (HL) and Primary mediastinal B cell lymphoma, total metabolic tumor volume (TMTV) or total lesion glycolysis (TLG) predicted outcome better than the bulk. From the H10 EORTC/LYSA/FIL randomized intergroup trial (NCT00433433) including patients with supradiaphragmatic stage I/II, histologically proven classical HL, we investigated the prognostic value of quantitative PET metrics measured on baseline FDG PET/CT in the unfavorable group of the standard arm.
Methods: One hundred and fifty patients were randomly selected from the 352 patients recruited by the LYSA centers, in the unfavorable group (≥ 4 nodal areas or age ≥ 50 yrs or mediastinal thoracic (MT) ratio ≥ 0.35 or erythrocyte sedimentation rate (ESR) ≥ 50 (without B-symptoms) or ESR ≥ 30 (with B-symptoms)) of the standard arm of the H10 trial. Only patients who had baseline PET/CT with fused images available were analyzed. Standard treatment was 4 cycles of ABVD completed by involved-node radiotherapy. All patients had an interim PET performed after 2 ABVD cycles (PET2). Baseline TMTV was computed using the 41% and 25% SUVmax thresholding methods; SUVmax, TLG41%, TLG25% were calculated. PET2 was centrally reviewed reported. Optimal quantitative parameters cut-off to predict PFS and OS were determined by ROC curves, and Kaplan Meier (KM) curves were obtained. Multivariate analyses were performed using a Cox model.
Results: 128 patients with a median age of 32 years were analyzed: 54 (42%) had B symptoms, 74 (58%) had ESR>40 (ROC optimal cut off), 48 (37%) mediastinal bulk as defined above. Median TMTV41%, TMTV25%, SUVmaxand TLG41%, TLG25% were 81 cm3 (25th-75thpercentiles 44-145 cm3), 194 cm3 (112-323), 11 (8-14), 407 cm3(221-475) and 731 cm3 430-1321) respectively. After a median follow-up of 5 years, the 5y-PFS was 84% and the 5y-OS was 92%.
The strongest PET quantitative parameter to predict outcome was the TLG41% (p=0.0006 HR=6.5 for PFS with a cut off of 420 cm3, p=0.025 HR=7.7 for OS with a cut off of 584 cm3). Patients with a high TLG41% had a 5y-PFS of 76% vs 92% (95%CI 71-81; 88-96) and a 5y-OS of 88% vs 96% (95%CI 83-92; 92-100) for those with the lower TLG41% respectively. Similar results were found using 25% SUVmax threshold (p=0.0005 HR=4.7 for PFS, p=0.0032 HR=7.9 for OS).
TMTV41% higher than 149 cm3 cut off was associated with a worse PFS (p=0.0099, HR=3.26) and OS (p=0.022, HR=4.8) but with a lower significance level. A SUVmax greater than 14 was also associated with a worse PFS (p=0.018 HR=3.0) with a 5y-PFS of 74% vs 86% but not with OS. In multivariate analysis testing TLG41% and SUVmax or TLG41%and TMTV41%, only TLG41% remained significant (p=0.0096 and p=0.015 for PFS and OS respectively).
B symptoms and ESR>40 were predictive of PFS (p=0.0077 HR=3.7 and p=0.0062 HR=6.07 respectively) but not of OS. MT ratio was predictive of neither PFS nor OS (p=0.49, p=0.20). In multivariate analysis, B symptoms, ESR>40 and TLG41% remained significant independent predictors of PFS (p=0.038; p=0.034; p=0.014 respectively).
For the 124 patients with a centralized reading available, a positive PET after two cycles (PET2 +) using IHP criteria (n=29) was associated with a worse PFS (p=0.0006). In multivariate analysis testing TLG41% and interim PET, they both remained independent prognosticators (p=0.014 and p=0.025 respectively).
Interestingly combining TLG41% and interim PET brings out 3 distinctive prognostic categories (p<0.0001): negative PET2 and low TLG41% with good outcome (5y-PFS=92%, n=60); positive PET2 and high TLG41% with bad outcome (5y-PFS=57%, n=21) and an intermediate category (5y-PFS=88%, n=43) cf. KM curve. No progression was observed in the 8 patients with a positive interim PET but a low baseline TLG41%, suggesting that TLG41% results may reduce the numbers of false positive PET2 patients.
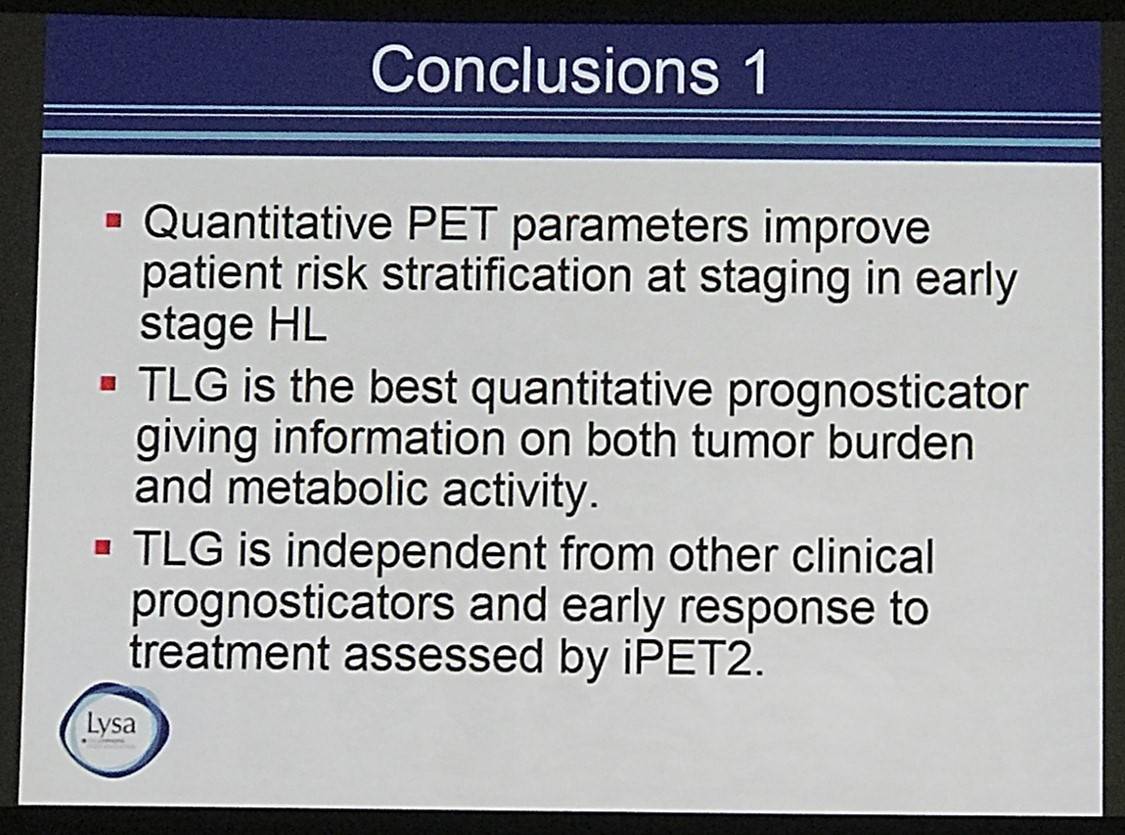
Conclusion: Quantitative PET parameters improve patient risk stratification at staging. The study data suggest that TLG is an independent prognosticator of outcome and seems particularly interesting in early stage HL patients, to identify in conjunction with the early PET response, those patients who require treatment intensification.
- Cottereau A.S. et al. Prognostic Value of Baseline Quantitative PET Metrics for Patients with Unfavourable Early Stage Hodgkin Lymphoma Enrolled in the Standard Arm of the EORTC/Lysa/FIL H10 Trial. 2016 December 3; Oral Abstract #184: ASH 58th Annual Meeting and Exposition, San Diego, CA.

Understanding your specialty helps us to deliver the most relevant and engaging content.
Please spare a moment to share yours.
Please select or type your specialty
 Thank you
Thank youNewsletter
Subscribe to get the best content related to lymphoma & CLL delivered to your inbox