All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the Lymphoma Coalition.
The Lymphoma Hub uses cookies on this website. They help us give you the best online experience. By continuing to use our website without changing your cookie settings, you agree to our use of cookies in accordance with our updated Cookie Policy
Introducing

Now you can personalise
your Lymphoma Hub experience!
Bookmark content to read later
Select your specific areas of interest
View content recommended for you
Find out moreThe Lymphoma Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the Lymphoma Hub cannot guarantee the accuracy of translated content. The Lymphoma Hub and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
ESMO 2016 | Selected Oral Presentations: DLBCL – HD-MTX is a highly effective prophylaxis in patients with high-risk of CNS relapse
Bookmark this article
Dr Teresa Calimeri from the San Raffaele Scientific Institute in Milan, Italy, and colleagues presented during the ESMO congress in October 2016 in Copenhagen, Denmark data from a retrospective study of 242 patients with Diffuse Large B-Cell Lymphoma (DLBCL), analyzing the effect of risk-tailored CNS prophylaxis with High-Dose Methotrexate (HD-MTX).
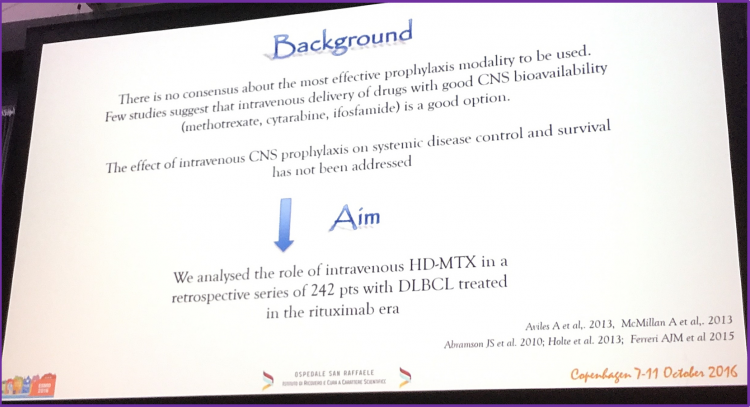
Patients were separated into two groups based upon their relative risk of CNS recurrence, with high-risk defined as either the involvement of specific extranodal organs and/or with an IPI score of 4–5. The prophylaxis schedule was methotrexate for 3–4 cycles intravenously with or without intrathecal chemotherapy (IT). Overall, 95 patients were in the high-risk group (39%) and 147 in the low-risk group (61%). Of the 95 patients in the high-risk group, 47 received no prophylaxis, 11 received IT alone and 36 received HD-MTX ± IT.
Patient Characteristics
| Low Risk (n = 147) | High Risk (n = 95) | |
|---|---|---|
| Median age | 66 (range 18-89) | 66 (range 24-89) |
| M/F ratio | 1.19 | 1.44 |
| PS<2 | 138 (94%) | 69 (73%) |
| B symptoms | 42 (29%) | 37 (39%) |
| Extranodal >1 | 5 (3.4%) | 42 (44%) |
| Bulky disease | 37 (25%) | 17 (18%) |
| Stage III-IV | 69 (47%) | 67 (71%) |
| IPI 0-3/4-5 | 147/- | 54/41 |
| Testis | - | 21 |
| Kidney/adrenal | - | 18 |
| Orbit | - | 6 |
| Breast | - | 1 |
| Paranasal/nasal | - | 8 |
| Skull/spine | - | 5 |
| Radiotherapy | 61 (41%) | 33 (35%) |
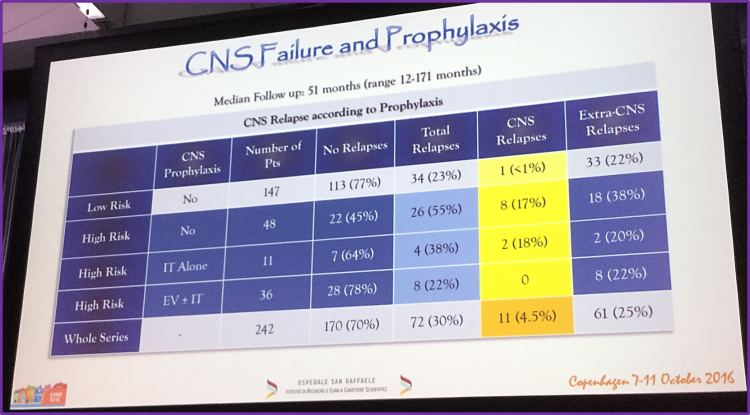
They reported that with a median follow-up time of 51 months, no one in the high-risk with HD-MTX ± IT prophylaxis group developed CNS relapse. However, two patients (18%) in the IT alone prophylaxis group, and 8 patients (17%) in the no prophylaxis group, developed CNS relapse.
Patient Outcomes - Responses After First-Line
| Low Risk (n = 147) | High Risk (n = 95) | |
|---|---|---|
| CR | 23 (84%) | 70 (74%) |
| PR | 2 (1%) | 4 (4%) |
| SD | 1 (0.7%) | 0 |
| PD | 19 (13%) | 19 (20%) |
| NA* | 2 (1.3%) | 2 (2%) |
*other causes of death: infections and heart failure
Reported three year PFS rates with HD-MTX ± IT were 81%, compared with 46% without HD-MTX. Three year OS rates were reported as 86% (HD-MTX ± IT), compared with 48% (without HD-MTX).
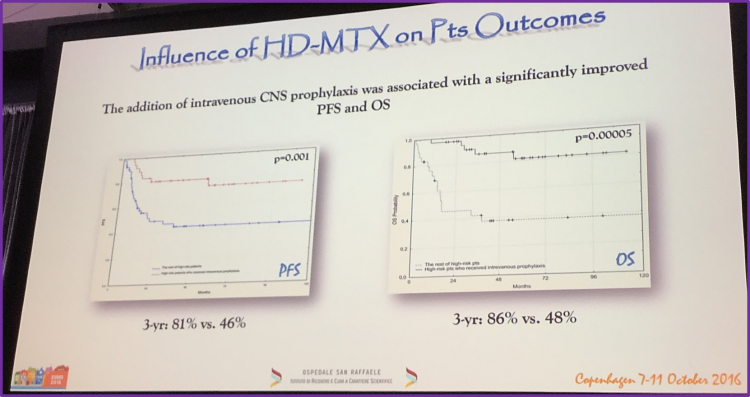
Their main conclusions at the end of this presentation were that combination prophylaxis with HD-MTX ± IT is highly effective in patients with DLBCL with high-risk of CNS relapse. They tempered this result by reminding the audience that this was a retrospective study and that the high mortality rates associated with CNS relapse could result in the reported OS effect.
Following this presentation, a discussion session was chaired by Professor Peter Johnson from the Faculty of Medicine, University of Southampton, UK. Data was presented on the risk of CNS relapse using either the IPI score or the involvement of specific extranodal organs, the two methods by which Calimeri T. et al. defined the high-risk group.
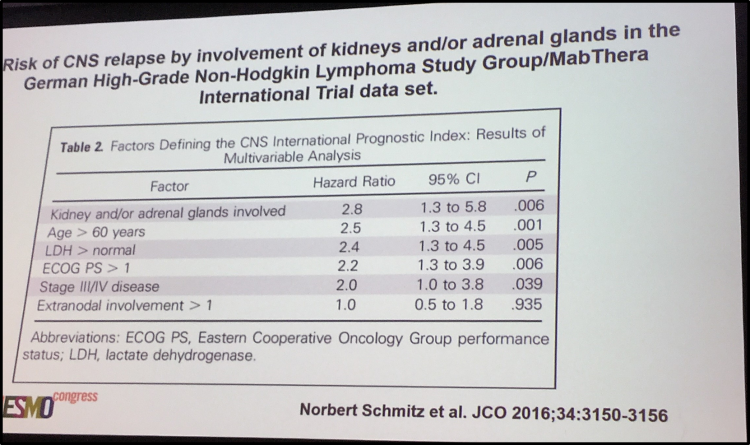

Prof. Peter Johnson then concluded by summarizing that IV MT-HDX is effective as prophylaxis in high-risk groups, the role of IT in this prophylaxis is unclear, however MT-HDX is most likely the best treatment option for patients in this group.
The talk concluded by stating that the evience remains unsatisfactory and is unlikely to improve greatly.
- Rituximab has reduced the risk of CNS recurrence
- High dose IV methotrexate is effective in high risk groups
- It is not clear whether IT prophylaxis contributes usefully
- In patients with adequate renal function and no other contraindications, high dose IV methotrexate is probably the treatment of choice

Understanding your specialty helps us to deliver the most relevant and engaging content.
Please spare a moment to share yours.
Please select or type your specialty
 Thank you
Thank youRelated articles
Newsletter
Subscribe to get the best content related to lymphoma & CLL delivered to your inbox








